Don’t Judge the Mouth Breather
Most of us don’t want to be judgmental people, but even the best of us make judgments on a daily basis. It’s a survival mechanism. We need to make judgements in order to protect ourselves from harm. For example, as much as I strive not to be judgmental or inconsiderate, I cannot bring myself to stop for hitchhikers.
We all make judgment calls every day and in some ways it’s essential to our survival. We judge whether the car driving down the road is going too fast for us to pull out into traffic before being rear-ended. We judge whether the food in the refrigerator has been there so long that it’s no longer safe to eat. (Sometimes Dr. Drews makes the wrong judgement on that one.)
Then there are those judgements we make that are based on information we think we know, but our information is somehow incomplete or inaccurate.

It is way too easy to judge the parent in Walmart whose kid is having a meltdown, but those sorts of judgements are often unfair!
True, there are parents who really could be better disciplinarians and “get control over their kid,” but there are also parents who struggle with behavior issues with their children that are in no way a result of poor (or lazy) parenting. ADHD, ODD, RAD, LMNOP. Ok, that last one is not a real thing, but with all the new psychological labels and disorders out there sometimes all the acronyms can get confusing.
OK, well, what does this have to do with dentistry?!
Let’s try some word association . . . The first word that comes to your mind when I say “ADHD” is often “naughty” or “uncontrollable.” And when I say, “obstructive sleep apnea,” people usually think of middle aged, overweight men with thick necks. While there are elements of truth to these associations, if we stopped there we would certainly have missed the mark.
Sleep Dentistry for Kids
Research is now showing us that sleep apnea occurs in children as well as adults, and its prevalence is increasing. It is estimated that 75% of patients suffering from sleep apnea have not been diagnosed*. In an earlier post this year I discussed the dangers of sleep apnea for adults. Now imagine how much more detrimental this can be for kids, for whom the functions of memory consolidation and emotional regulation are essential to their development.
What are the symptoms of ADHD? Hyperactivity, difficulty focusing, easily distracted, poor schoolwork, sometimes aggressive or grouchy behavior. I don’t know about you, but when I was a child I had those exact same symptoms – when I was overtired! If a child is never able to achieve a good night’s sleep because he cannot breathe properly when he is sleeping, these same symptoms rear their ugly heads.
I am certainly not suggesting that all kids with letter disorders (ADHD, ODD, RAD, etc.) are really suffering from sleep apnea, but there are many studies in the literature indicating that there is a fair amount of misdiagnosis occurring.
A 2004 study indicated that 50% of children with ADHD showed evidence of sleep disordered breathing**. A large study of over 11,000 children indicated that among children with sleep disordered breathing, 40-100% showed symptoms mimicking ADHD by 7 years of age***.
Signs of Sleep Disordered Breathing in Children
A child may be at increased risk for sleep disorders if she has enlarged tonsils and adenoids. The size of these structures relative to the child’s airway is key. Habitual snoring is a huge red flag here.
Children should not be snoring; and if they are, then this is reason enough to investigate their sleep patterns. 50% of children who snore are diagnosed with obstructive sleep apnea.**** The rate of sleep disordered breathing in children is on the rise, at a similar rate as obesity, in fact. In fact, a child with a BMI in the obese range would be significantly more likely to suffer from sleep apnea.
What type of symptoms do these children manifest?
The stupid-lazy child who frequently suffers from headaches at school, breathes through his mouth instead of his nose, snores and is restless at night, and wakes up with a dry mouth in the morning, is well worthy of the solicitous attention of the school medical officer. This nineteenth- century reference was published in an article entitled ‘On some causes of backwardness and stupidity in children’ and describes the unfortunate sequelae resulting from lack of recognition and treatment for the common disease we now know as the pediatric obstructive sleep apnea syndrome (OSAS).^
As evidenced above, when we make judgments about children based on their behavior without having all the facts, it can create very negative labels that are both unfair and inaccurate. Nowadays, you’d never see a child with these symptoms labeled as “lazy-stupid,” but you may see him labeled as “defiant” or “hyperactive,” when really he just needs a good night’s sleep. Other symptoms these kids can exhibit are increased ear infections, respiratory infections, bruxism (grinding teeth), and enuresis (bedwetting).
Cardiopulmonary problems like hypertension (high blood pressure), heart attack, and stroke are more common in the adult sleep apnea population, but in extreme cases these can affect children as well. I think it’s important to note here that while nocturnal bruxism can be a symptom of sleep disordered breathing in kids, not ALL kids who grind their teeth have this problem. But if the child is a grinder AND a mouth breather, it would be prudent to investigate her tonsils and adenoids because this is a good indication there may be a need for intervention.
Children with sleep disordered breathing will grow differently as well. Children with large tonsils and adenoids will often breathe through their mouths to compensate for a lack of air through their nose. This creates a problem, however, because the air you breathe through your nose produces nitric oxide which helps to dilate blood vessels and allows a greater rate of oxygen absorption into the tissues. Breathing through the mouth does not provide this same function, and as a result the child is working harder to breathe, and receiving less oxygen in the process. This results in decreased brain development, particularly in the areas responsible for decision making and reasoning.
Additionally, if the nasal sinuses are not being adequately exercised they don’t develop properly, resulting in a narrower palate or upper jaw, which then causes crowded teeth. Sometimes these kids have longer lower faces because of the way their jaws hang open for mouth breathing. Their tongues grow larger and wider. In fact, there are many adults I see with sleep issues which could have potentially been treated preventatively when they were children to lessen the severity of their facial abnormalities and their apnea symptoms if someone had intervened earlier.
Treatment for Sleep Disordered Breathing in Children
So what do we do to help these kids?
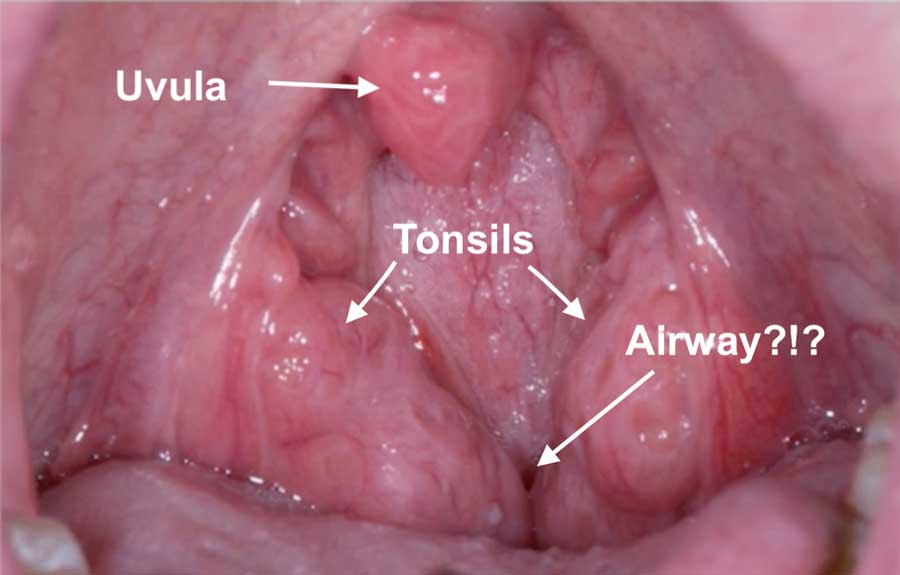
It starts with evaluating their tonsils and adenoids. When a patient comes into the dental office we have her stick out her tongue and say, “Ah.” On occasion, this is what we’ll see:
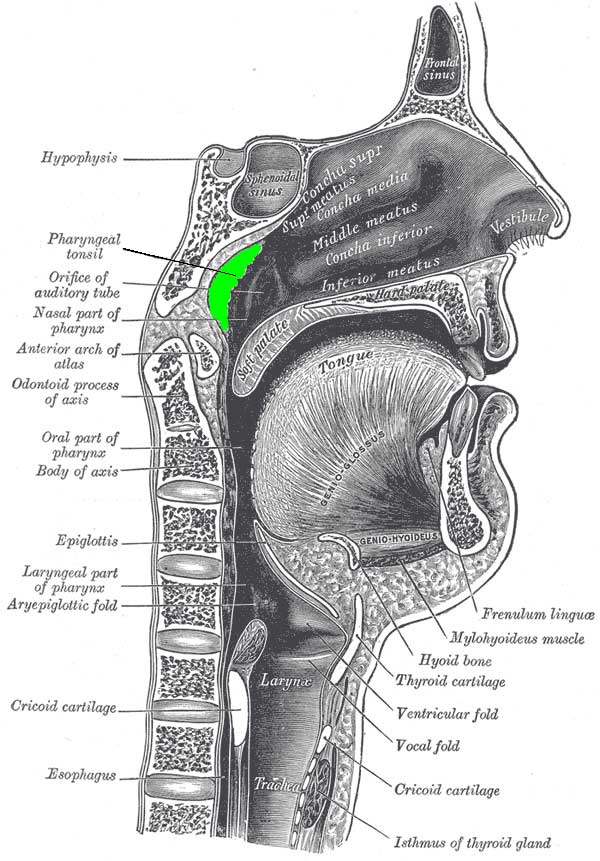
When I see tonsils this large, my first recommendation is that the parent follow up with an ENT for evaluation of tonsils and adenoids for removal. I am unable to visualize the adenoids from my perspective, but the ENT will have more access. The adenoids are located behind the nasal cavity before the airway meets up with the throat. They are also known as “pharyngeal tonsils” and when they are large or inflamed it’s obvious to see how that could create a compromise in the patient’s airflow.
Removing the adenoids and tonsils results in an 80-90% cure rate for sleep apnea in most children. In children with obesity, however, that number shrinks down to 50%. For these kids, a CPAP machine is the way to go. There has even been evidence that treatment with a CPAP machine will help increase metabolism, thereby helping to treat the obesity as well as the sleep apnea. A 2003 study found that after just 2 days of CPAP treatment, insulin sensitivity improved and this effect was sustained at 3 months.^^
Treating Obstructive Sleep Apnea as early as possible provides the child with a better chance for healthy, normal development of the oral maxillofacial region, and prevents further, more invasive treatments down the road. It can prevent this issue from persisting into adulthood, which could save the person’s life. Less significantly, from a dental perspective, it can certainly prevent more expensive orthodontic treatment if the child is able to develop properly and not develop a large tongue and narrow palate.
What about treating the child who simply grinds his teeth at night?
Many children who grind their teeth will simply grow out of it. Treating a child with a night guard is very difficult, as their dentition is constantly changing and their jaws are growing. We do not treat children with bruxism by fabricating an occlusal splint as we do for adults because it’s not necessary, and it can actually restrict growth if fabricated too early. For those children who do not outgrow their grinding habit, we can certainly treat them with a night guard once they have completed their growth spurts and have fully developed their adult dentition.
We all remember the snotty-nosed, mouth-breathing kids in our classes in elementary school. Looking back at it, some of them were a little bit less “with it” than the rest of us, and now we know why. And those kids throwing themselves on the floor in Walmart while we’re trying to complete our last minute Christmas shopping are potentially going through more than we realize! Maybe they haven’t been able to get a good night’s sleep in a very long time.
Let’s all make a New Year’s Resolution to judge a little less and educate a little more.
Here’s wishing you a very Merry Christmas and Happy New Year!
Love & Mouth Breathing,
Kristie Lake, DMD
Resources
*Perez, Cristina “Obstructive Sleep Apnea Syndrome in Children.” General Dentistry. 2018 November/December; 66(6):46-50.
**Golan, N. et al. “Sleep Disorders and Daytime Sleepiness in Children with Attention Deficit Disorder.” Sleep. 2004 Mar 15;27(2):261-6.
***Bonuck, Karen et al. “Sleep-Disordered Breathing in a Population-Based Cohort: Behavioral Outcomes at 4 and 7 Years” Pediatrics, April 2012, Volume 129/Issue 4
****Trosman, I. “Childhood Obstructive Sleep Apnea Syndrome: A Review of the 2012 American Academy of Pediatrics Guidelines.” Pediatr Ann. 2013 Oct;42(10):195-199
^Arali, Veena et al. “Pediatric Obstructive Sleep Apnea Syndrome: Time to Wake Up.” Int J Pediatric Dentistry. 2012 Jan-Apr; 5(1): 54–60.
^^ Harsch, IA et al. “Continuous Positive Airway Pressure Treatment Rapidly Improves Insulin Sensitivity in Patients with Obstructive Sleep Apnea Syndrome.” Am J Resp Crit Care Med. 2004;169:156-162